For decades, the fight against cancer has relied on a three-pronged approach: surgery, radiation, and chemotherapy. While these treatments have saved countless lives, they often come with harsh side effects and limited effectiveness for certain cancers. However, a new wave of innovation is transforming the landscape – immunotherapy.
Unleashing the Body’s Defenders: How Immunotherapy Works?
For centuries, the human body’s immune system has been our first line of defense against invaders, from viruses to bacteria. But cancer cells, with their ability to camouflage and evade detection, have posed a formidable challenge.
Immunotherapy harnesses the innate power of the body’s immune system to identify and eliminate cancer cells. This revolutionary approach operates through two primary methods: bolstering the immune system’s capabilities to enhance its ability to combat cancer cells or selectively targeting and neutralising specific proteins, known as receptors, on cancer cells to thwart their evasion tactics against the immune system. Knowing the power of immune cells, the next question is, can immunotherapy cure all cancers?
What Are the Types of Immunotherapy and what specific cancer can it potentially cure?
1. Checkpoint Inhibitors in Cancer Immunotherapy
Our immune system has a natural way of keeping itself in check. These checkpoints prevent the immune system from going into overdrive and attacking healthy tissues. However, cancer cells can exploit these checkpoints to evade immune attack.
Immune checkpoint inhibitors are drugs that target these checkpoints, blocking the cancer cells’ ability to hide from the immune system. This allows the immune system to recognise and destroy cancer cells more effectively.
Inhibitors targeting the Programmed cell death protein-1/ligand 1 (PD-1/L1) pathway are a prominent example. These drugs operate by blocking the interaction between two key proteins: PD-1, located on T cells, and PD-L1, found on both cancerous and some healthy cells. When PD-1 binds to PD-L1, it signals the T cell to cease its attack. By blocking PD-1 or PD-L1, these drugs allow T cells to continue attacking cancer cells.
Here are a few examples of immune checkpoint inhibitors:
- Pembrolizumab (Keytruda): A PD-1 inhibitor approved for the treatment of various cancers, including melanoma, lung cancer, and bladder cancer.
- Nivolumab (Opdivo): Another PD-1 inhibitor with similar approvals to pembrolizumab.
- Atezolizumab (Tecentriq): A PD-L1 inhibitor approved for the treatment of several types of cancer, including bladder cancer and non-small cell lung cancer.
2. Adoptive Cell Therapy (ACT) in Cancer Immunotherapy
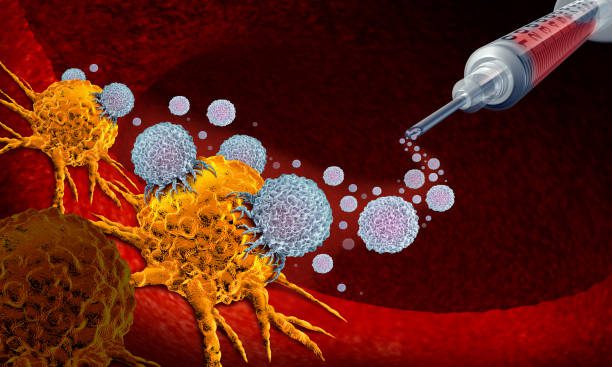
Unlike immune checkpoint inhibitors that broadly stimulate the immune system, ACT takes a more targeted approach. This personalized approach involves engineering a patient’s immune cells, typically T cells, to recognise and attack their specific cancer cells. The T cells are then reintroduced into the patient’s body, where they can launch a targeted attack on the cancer.
There are several variations of ACT, each with its own strengths. CAR T cell therapy is a rapidly evolving and highly effective form of ACT. In this approach, T cells are engineered with a special receptor (CAR) that allows them to recognise and attack specific proteins on the surface of cancer cells. CAR T cell therapy has shown remarkable results in treating certain blood cancers.
Another ACT approach is tumour-infiltrating lymphocyte (TIL) therapy. This method leverages T cells that have already infiltrated the patient’s tumour. These TILs are extracted, expanded in the lab, and then reintroduced into the patient. TIL therapy can be effective for some solid tumours.
Natural killer (NK) cell therapy is a newer approach that utilises natural killer cells, another type of immune cell, to fight cancer. NK cells have the inherent ability to recognise and attack cancer cells without any prior exposure. Researchers are currently exploring the use of CAR technology to enhance the effectiveness of NK cells against cancer, creating CAR NK cells.
3. Therapeutic Cancer Vaccines in Cancer Immunotherapy
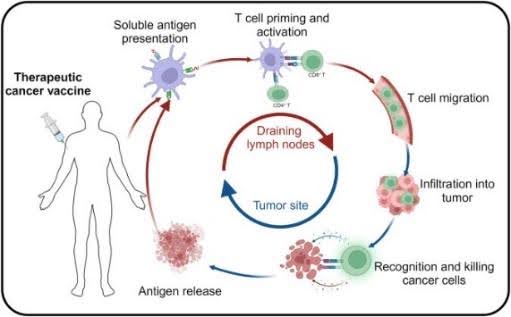
Unlike traditional vaccines, which prevent infectious diseases by priming the immune system to recognise specific pathogens, therapeutic cancer vaccines aim to stimulate the immune response against existing cancer cells.
These vaccines typically work by introducing specific cancer-related antigens or fragments of cancer cells into the body. These antigens are recognised by the immune system as foreign, triggering an immune response targeted at eliminating cells displaying those antigens.
Therapeutic cancer vaccines can be tailored to target specific types of cancer or even personalised to an individual’s unique tumour antigens. They may be used alone or in combination with other cancer treatments, such as chemotherapy, radiation therapy, or immunotherapy drugs.
For example, Sipuleucel-T is the first FDA-approved therapeutic vaccine for advanced prostate cancer. It targets prostate acid phosphatase (PAP), a protein expressed by prostate cancer cells. The vaccine stimulates the patient’s immune system to produce PAP-specific T cells, which can recognise and destroy PAP-positive cancer cells. This vaccine consists of a fusion protein combining recombinant PAP with granulocyte-macrophage colony-stimulating factor (GM-CSF), which activates antigen-presenting cells (APCs) within the autologous peripheral blood mononuclear cells (PBMC). Subsequently the cells are infused back to the patient to induce the replication of PAP-specific T cells.
4. Monoclonal Antibody Therapy in Cancer Immunotherapy
Monoclonal antibodies are lab-made antibodies to home in on specific proteins found on cancer cells. Once attached, monoclonal antibodies can unleash a multi-pronged attack on cancer in several ways:
- Triggering immune response: They can directly stimulate the immune system to recognise and destroy the cancer cell.
- Blocking growth signals: Some monoclonal antibodies bind to receptors on cancer cells that normally receive signals to grow and divide. By blocking these signals, they halt the cancer cells’ growth.
- Flagging for destruction: Certain monoclonal antibodies act like flags, attracting immune system cells like macrophages that engulf and destroy the cancer cell.
This targeted approach offers a significant advantage in cancer treatment. Unlike traditional chemotherapy drugs that can harm healthy cells along with cancer cells, monoclonal antibodies can more precisely target cancer with minimal side effects on healthy tissues. This translates to a more tolerable treatment experience for patients.
Here are a few examples of monoclonal antibody therapies:
- Trastuzumab (Herceptin): This monoclonal antibody targets the HER2 protein, which is overexpressed in some breast and stomach cancers. Trastuzumab has significantly improved outcomes for patients with HER2-positive breast cancer.
- Cetuximab (Erbitux): This monoclonal antibody targets a protein called EGFR, which is found on some head and neck cancers and colorectal cancers. Cetuximab can block tumour growth and is often used in combination with other therapies.
5. Cytokines Therapy in Cancer Immunotherapy
Cytokines are vital small protein molecules released by immune cells to transmit signals to other cells, typically triggered by threats or activating events such as infections. Various cytokines can prompt immune cells to mature, develop cell-killing functions, proliferate, or migrate throughout the body. Conversely, they may also attenuate the immune response to restrict tissue damage or terminate the immune reaction once the targeted threat or infection is eliminated.
One prominent example of cytokine application in therapy is interferon-alpha (IFN-α), which has been discovered to augment anti-cancer immune functions, induce cancer cell death in certain cancers, and hinder the formation of blood vessels in some solid tumours. Another significant cytokine utilised in therapy is Interleukin-2 (IL-2), which fosters the proliferation and activation of T cells and NK cells responsible for killing cancer cells. Despite the promising therapeutic potential of these cytokines, a significant challenge remains in delivering them effectively to specific cells while minimising side effects. Researchers are exploring innovative strategies such as utilising nanocarriers to achieve precise and targeted delivery.
A Work in Progress with Exciting Potential
Immunotherapy is a rapidly evolving field with immense promise. While not a one-size-fits-all solution, it offers a new wave of hope for cancer patients. Researchers are constantly exploring new approaches and combination therapies to overcome resistance and personalise treatment plans. The future of cancer treatment is likely to be a symphony of multiple approaches, with immunotherapy playing a leading role.
The Challenges and Future of Immunotherapy
While the potential for a cure is exciting, there are still hurdles to overcome. One major challenge is tumour resistance. Cancer cells are adept at evolving and developing mechanisms to escape immune attack. Researchers are actively investigating ways to overcome this resistance, including combining immunotherapy with other treatment modalities or developing strategies to target different immune checkpoints simultaneously.
Another significant challenge is personalising immunotherapy for each patient. Cancers are complex and vary greatly between individuals. Developing therapies that effectively target a patient’s specific cancer mutation profile is crucial for maximizing efficacy. This requires continued advancements in tumour profiling and the ability to tailor immunotherapies to an individual’s unique immune response.
A Final Note
It’s important to remember that immunotherapy is still evolving, and not every patient will experience a complete cure. However, the potential for long-term remission and improved quality of life is a significant advancement in the fight against cancer. As immunotherapy continues to develop, we can move closer to a future where cancer is not just a disease to be managed, but one that can be truly eradicated.
References
Berraondo P, Sanmamed MF, Ochoa MC, et al. Cytokines in clinical cancer immunotherapy. Br J Cancer. 2019;120(1):6-15. doi:10.1038/s41416-018-0328-y
Cheever MA, Higano CS. PROVENGE (Sipuleucel-T) in prostate cancer: the first FDA-approved therapeutic cancer vaccine. Clin Cancer Res. 2011;17(11):3520-3526. doi:10.1158/1078-0432.CCR-10-3126
Chen Y, Pei Y, Luo J, Huang Z, Yu J, Meng X. Looking for the Optimal PD-1/PD-L1 Inhibitor in Cancer Treatment: A Comparison in Basic Structure, Function, and Clinical Practice. Front Immunol. 2020 May 29;11:1088. doi: 10.3389/fimmu.2020.01088.
Delgado M, Garcia-Sanz JA. Therapeutic Monoclonal Antibodies against Cancer: Present and Future. Cells. 2023 Dec 14;12(24):2837. doi: 10.3390/cells12242837.
Fan T, Zhang M, Yang J, Zhu Z, Cao W, Dong C. Therapeutic cancer vaccines: advancements, challenges, and prospects. Signal Transduct Target Ther. 2023 Dec 13;8(1):450. doi: 10.1038/s41392-023-01674-3.
Yang M, Olaoba OT, Zhang C, Kimchi ET, Staveley-O’Carroll KF, Li G. Cancer Immunotherapy and Delivery System: An Update. Pharmaceutics. 2022 Aug 4;14(8):1630. doi: 10.3390/pharmaceutics14081630. PMID: 36015256; PMCID: PMC9413869.